
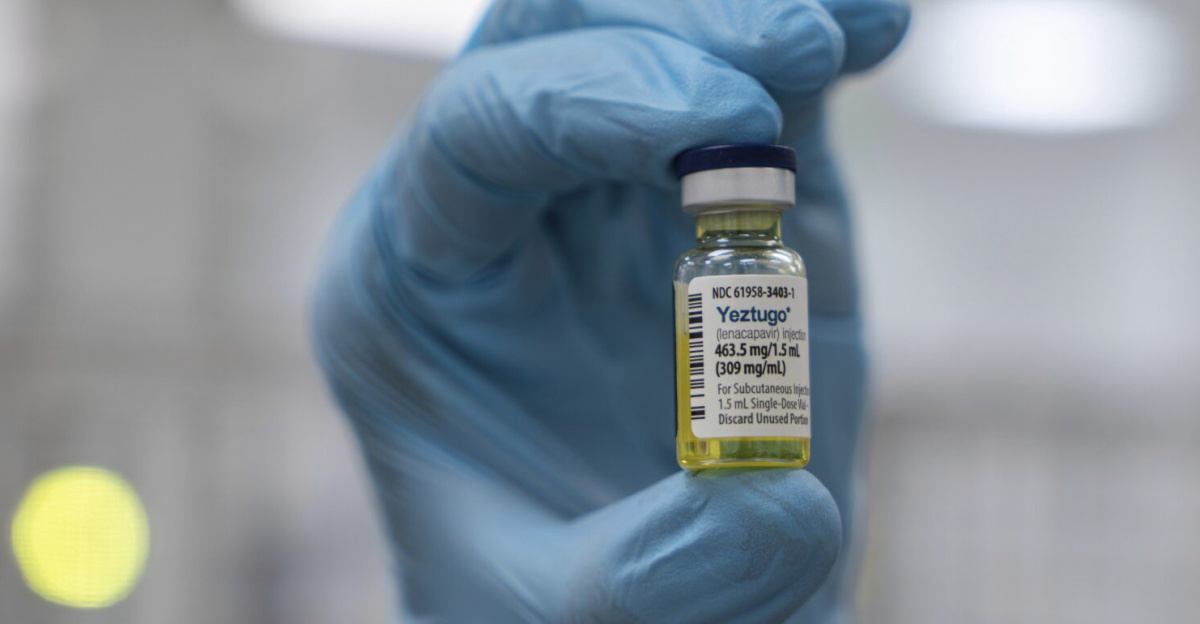
In June 2025, global HIV prevention reached a historic milestone. Gilead Sciences announced that the U.S. Food and Drug Administration had approved Yeztugo, the brand name for lenacapavir, as the first and only twice‑yearly injection proven to block nearly all sexually acquired HIV infections.
According to Phase 3 trial data published in The New England Journal of Medicine, more than 99.9% of participants remained HIV‑negative, an efficacy unmatched in the history of HIV prevention. Experts say this may be the first realistic opportunity to end new infections entirely, moving beyond decades of strategies aimed only at slowing transmission.
Global Endorsement and WHO Guidance

In July 2025, the World Health Organization called on governments worldwide to integrate twice‑yearly injectable lenacapavir into national HIV prevention programs as a preferred PrEP option. WHO Director‑General Dr. Tedros Adhanom Ghebreyesus said, “While an HIV vaccine remains elusive, lenacapavir is the next best thing – a long‑acting antiretroviral shown to prevent almost all HIV infections among those at risk.”
This guidance follows four decades of gradual advances in HIV prevention. It marks the clearest indication yet from global health leaders that a tool now exists with the potential to alter the course of the epidemic.
How Lenacapavir Works
Lenacapavir belongs to a new class of drugs known as capsid inhibitors. It targets the virus’s protein shell, or capsid, disrupting essential steps in HIV replication. This prevents the virus from entering and infecting healthy cells.
Its molecular design enables an exceptionally slow release into the bloodstream, allowing protection for up to six months from a single subcutaneous injection. According to Gilead researchers, this long‑acting mechanism was the breakthrough that took two decades to perfect.
Until now, no HIV medicine – treatment or prevention – has been able to provide such extended protection from one dose.
Unprecedented Efficacy in Clinical Trials

The pivotal PURPOSE 1 and PURPOSE 2 Phase 3 trials enrolled thousands of participants across Africa, the Americas, and Asia. In both studies, there were zero new HIV infections among those receiving lenacapavir.
University of Cape Town scientist Linda‑Gail Bekker described the results as “spectacular,” noting that trials were stopped early due to overwhelming efficacy.
The studies compared lenacapavir to daily oral PrEP regimens, which require strict adherence, and found the injectable was 100% effective in one high‑risk group. The findings confirmed the drug’s effectiveness across diverse populations, including young women in high‑incidence regions.
A Historic Recognition in Science

In December 2024, Science magazine named lenacapavir its “Breakthrough of the Year.” Stephen Yant, vice president of virology research at Gilead Sciences, said the journey to the drug’s final form was “always one atom away” from failure, with the team facing multiple setbacks before achieving a potent and stable molecule for twice‑yearly dosing.
The award marked a pharmaceutical milestone and recognition of the persistent, methodical research that began in the early 2000s and ultimately produced one of the most essential HIV prevention tools to date.
Solving the Adherence Problem

Daily HIV prevention pills, while up to 99% effective in ideal conditions, have been far less effective in real‑world settings. A 2022 study in The Lancet HIV reported protection dropping to as low as 26% among groups unable to maintain daily adherence. Reasons ranged from stigma to pill fatigue to inconsistent healthcare access.
By requiring only two doses per year, lenacapavir removes the primary barrier to oral PrEP success. Public health officials say this simple shift could dramatically change outcomes for communities where daily pill use has failed to curb new infections.
Impact on Sub‑Saharan Africa
Sub‑Saharan Africa, where young women and adolescent girls remain disproportionately affected by HIV, stands to gain significantly. According to UNAIDS, women aged 15–24 accounted for 77% of new infections in this age group in the region in 2023. Stigma, gender inequality, and healthcare access gaps have limited uptake of daily PrEP.
The appeal of two discreet injections per year could overcome these barriers. UNAIDS Executive Director Winnie Byanyima has emphasized that the promise of lenacapavir will only be realized if it is made affordable and accessible to at-risk populations.
Momentum at the 2025 IAS Conference

The 13th International AIDS Society Conference, held in Kigali, Rwanda, in July 2025, became a rallying point for long‑acting HIV prevention strategies. Rwanda’s Minister of Health, Dr. Sabin Nsanzimana, credited people‑centred approaches and strategic partnerships with helping the country achieve the UNAIDS 95‑95‑95 targets.
Delegates from more than 150 countries discussed how lessons from Rwanda’s HIV response could be applied to the rapid rollout of lenacapavir in similar settings. The conference marked a shift from cautious optimism to concrete planning for global adoption.
WHO’s New Prevention Standard

WHO’s updated guidelines position lenacapavir alongside existing oral PrEP and the monthly dapivirine vaginal ring, but place special emphasis on its twice‑yearly schedule as a game‑changer for populations with adherence challenges.
Dr. Meg Doherty, WHO’s Director of Global HIV, Hepatitis, and STIs Programmes, said the organization would “work with governments, manufacturers, and donors to ensure communities gain access quickly.” Public health experts note that the guidelines also call for targeted rollout, prioritizing individuals and regions with the highest HIV incidence.
Real‑World Rollout Plans
Health ministries are already preparing to integrate lenacapavir into national prevention programs. In South Africa, the National Department of Health has announced plans to offer the injections at public clinics, mobile outreach sites, and select pharmacies. Trial data show most side effects are mild, such as temporary injection site pain.
Training programs for nurses and community health workers are underway to ensure safe administration. Experts say early rollout will test health systems’ ability to deliver biannual care consistently, a new logistical challenge for HIV prevention.
Cost and Access Concerns

The price of lenacapavir remains a pressing question. While Gilead has pledged to work with global health partners, UNAIDS has called for significant price reductions to avoid creating a new barrier to prevention. According to Médecins Sans Frontières, high drug costs have historically slowed access to lifesaving HIV treatments in low‑income countries.
Funding from initiatives such as the Global Fund and the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) will ensure that lenacapavir reaches those who need it most, rather than remaining concentrated in high‑income markets.
Integrating Into Existing HIV Programs

Public health agencies emphasize that lenacapavir must be incorporated into broader prevention strategies rather than replace them. Combining it with HIV testing, sexual health education, and condom distribution will maximize impact. Dr. Nittaya Phanuphak of the Institute of HIV Research and Innovation in Bangkok noted that layered prevention is essential to address varying needs across populations.
Integration will also help sustain engagement with healthcare providers, ensuring that prevention remains part of a continuum of care that includes early diagnosis and treatment.
Advances in HIV Treatment

While lenacapavir represents a breakthrough in prevention, parallel progress is being made in treatment. Gene‑editing tools like CRISPR and immune‑based therapies are promising in small studies, with some individuals maintaining viral suppression after stopping antiretroviral drugs.
In March 2025, researchers at the University of California, San Francisco, reported long‑term remission in a patient treated with a combination of immune modulation and stem cell transplantation. Though a scalable cure remains out of reach, experts say prevention advances and treatment innovations are moving the field closer to ending the epidemic.
Lessons From Two Decades of Research

The path to lenacapavir was anything but certain. Internal accounts at Gilead describe a project that nearly collapsed multiple times due to molecular instability and manufacturing hurdles. “Management had difficulty killing the project,” one scientist told Science, noting how it endured despite shifting corporate priorities.
The final molecule’s long‑acting properties were achieved only after hundreds of failed candidates. Researchers say the drug’s approval underscores the importance of sustained investment in basic Science, even when immediate results seem uncertain.
Tracking the Epidemic in 2025

As of mid‑2025, seven countries have met the UNAIDS 95‑95‑95 targets: 95% of people with HIV knowing their status, 95% of those on treatment, and 95% achieving viral suppression. Despite this progress, UNAIDS reports more than 1 million new infections annually, with Eastern Europe and Central Asia seeing increases linked to gaps in harm reduction services.
Global health officials warn that the introduction of lenacapavir must be matched by continued investment in testing, treatment, and public health infrastructure to prevent a resurgence of the virus.
Preparing Healthcare Providers

In anticipation of wider availability, healthcare providers are trained to identify candidates for lenacapavir, manage dosing schedules, and monitor outcomes. In the U.S., the Centers for Disease Control and Prevention is developing educational materials for clinicians on integrating the drug into routine care.
Providers in rural and underserved areas say the biannual schedule could improve outreach to patients who travel long distances for care or face stigma that deters frequent clinic visits.
Patient Experience and Community Response

Patient advocates report strong enthusiasm for the new option. In Kenya, participants from trial sites told The Guardian that biannual injections eased anxiety over missed doses and allowed them to feel normal without the daily reminder of HIV risk.
Community organizations stress that choice is essential; some may still prefer oral PrEP or other methods. The introduction of lenacapavir is seen as expanding, rather than replacing, the prevention toolbox, empowering individuals to choose the method that best fits their lives.
Industry and Research Perspectives
Pharmaceutical leaders view lenacapavir’s approval as proof that long‑term investment in HIV science yields transformative returns. Researchers are already exploring next‑generation capsid inhibitors and experimental injectables lasting up to a year.
Dr. Anthony Fauci, former director of the U.S. National Institute of Allergy and Infectious Diseases, told STAT News that lenacapavir’s success sets a precedent for thinking big in infectious disease prevention. Industry observers believe the technology could eventually be adapted for other chronic viral infections.
Remaining Challenges and Policy Goals

Despite optimism, experts caution that scientific breakthroughs alone cannot end HIV. Legal and policy barriers, such as laws criminalizing same‑sex relationships or drug use, continue to hinder prevention efforts in many countries.
WHO and UNAIDS are urging governments to pair lenacapavir rollout with human rights protection, expanded harm reduction, and increased funding for community‑led programs.
Advocates say that each dollar invested in HIV prevention strengthens broader health systems, improving resilience against future public health threats.
A New Era in the Journey to End HIV

With lenacapavir’s launch, the global health community stands at a decisive moment. For the first time, a future without new HIV infections appears within reach. Achieving it will depend on governments, health agencies, and communities translating scientific success into universal access.
As Dr. Tedros said, “We have the tools to end HIV as a public health threat; what remains is the collective will to use them.” The next few years will determine whether this milestone becomes a turning point or a missed opportunity.






